The United States is in the grip of the worst drug overdose epidemic in its history; a catastrophe fueled not by a virus or a natural disaster, but by human avarice and institutional failure. A federal judge overseeing opioid litigation aptly described it as “a man-made plague, 20 years in the making” (1). Since 2000, more than one million Americans have died from drug overdoses, the majority caused by opioids (2). This crisis was entirely avoidable: it began with pharmaceutical companies aggressively pushing potent opioids for profit, was enabled by asleep-at-the-wheel regulators, and evolved as crackdowns on pills gave rise to a flood of heroin and illicit fentanyl. The result has been a public health calamity that has devastated families, destroyed communities, and left urban neighborhoods blighted by addiction. What follows is a chronological investigation of the actors and events that created the opioid nightmare; a blunt accounting of how corporate greed, regulatory incompetence, and criminal opportunism converged to unleash unprecedented suffering.
Purdue Pharma and the OxyContin Offensive
In the mid-1990s, Purdue Pharma; owned by the Sackler family; launched OxyContin, a new extended-release oxycodone pill. It was a calculated quest for profit: Purdue had learned that long-acting opioids could be a goldmine if marketed as safe for common pain. In 1995, the FDA approved OxyContin for moderate-to-severe pain, remarkably allowing Purdue to claim on the drug’s label that addiction to opioid painkillers was “very rare” when used properly. The label even suggested that OxyContin’s delayed absorption was “believed to reduce the abuse liability” of the drug; a claim with no scientific basis, which gave Purdue a green light to assure doctors the drug was less addictive (4). Armed with this federal blessing, Purdue mounted an unprecedented marketing blitz. The company doubled its sales force and showered physicians with glossy brochures, free coupons, and promotional swag (hats, tote bags, even OxyContin-branded CD music samples), all repeating the lie that opioid addiction was unlikely (4). Sales reps were trained to minimize doctors’ fears; they falsely asserted that OxyContin produced no euphoric high and caused no withdrawal symptoms; outright fabrications designed to overcome reluctance to prescribe a powerful opioid (3). As one U.S. Attorney later summarized, “OxyContin was the child of marketers and bottom-line financial decision-making,” not of medical science (3).
The results were as lucrative as they were lethal. Purdue’s aggressive marketing paid off in a surge of prescriptions: OxyContin sales exploded from about $48 million in 1996 to over $1.1 billion by the year 2000 (4). The drug was being handed out for all manner of aches and injuries, far beyond the cancer patients it was originally meant for. This flood of pills sparked a parallel surge in abuse and addiction. By 2004; less than a decade after its introduction; OxyContin had become one of the country’s most widely misused drugs, a staple on the black market and a scourge in rural Appalachia and other regions (4). Internal Purdue documents (unearthed years later) showed the Sackler family and executives knew early on about reports of OxyContin being crushed, snorted, and stolen, yet they continued to expand sales. The company’s mantra, “pain is undertreated,” cloaked a ruthless strategy to sell as much opioid as possible. Purdue incentivized high prescribing with lavish bonuses and even targeted “super-prescriber” doctors who doled out enormous quantities, including flagrant pill-mill operators. All the while, the Sacklers were reaping a fortune. Even after Purdue’s misconduct began coming to light, the Sackler family extracted over $10 billion from Purdue’s opioid profits between 2008 and 2017, funneling the money into trusts and overseas accounts (12). They cashed in while the epidemic of addiction they stoked engulfed American communities. In 2007, Purdue Pharma and three of its executives pleaded guilty in federal court to criminal charges of “misbranding” OxyContin and deceiving regulators and doctors about its addiction risks. Purdue paid $600 million in fines (a slap on the wrist given its revenues), and no one went to prison (3). The company’s official confession acknowledged that some employees had intentionally misled the medical community. But by then the damage was done; Purdue’s campaign of lies had already sown the seeds of a nationwide catastrophe.
Regulatory Failures: FDA and Government in the Pocket
The Food and Drug Administration (FDA); the agency charged with protecting public health; utterly failed to blow the whistle on the unfolding opioid disaster. In fact, FDA decisions actively enabled it. Approving OxyContin’s overly broad label in 1995 (with its false claims about low addiction risk) was the first egregious mistake. Even after reports of abuse poured in, the FDA was sluggish to act; it was not until 2001 that the agency finally forced Purdue to change OxyContin’s label, deleting the bogus “abuse deterrence” claim and warning of addiction; too late to un-ring the bell (4). Over the next decade, as prescription opioids flooded the country, the FDA and other regulators remained largely ineffectual, exhibiting what can only be described as regulatory capture and willful blindness. A presidential commission in 2017 identified “inadequate oversight by the Food and Drug Administration” as one cause of the opioid crisis (1). The FDA’s own former commissioner has publicly admitted the agency “was wrong” in allowing opioid makers to promote long-term use for chronic pain, a use never properly validated (1). Yet the FDA did little to rein in opioid marketing or require more rigorous proof of safety. By all accounts, the FDA’s opioid regulators were too cozy with industry; exemplified by an FDA medical reviewer who left the agency to take a lucrative job at Purdue shortly after OxyContin’s approval. The result was a watchdog that barely barked while opioid pills were handed out like candy. This dereliction of duty by the FDA allowed Purdue and its peers to spread disinformation virtually unchecked (1).
Other government actors were likewise asleep at the switch or, worse, complicit. The Drug Enforcement Administration (DEA); responsible for monitoring controlled substances; failed to stop obvious diversion of opioids to the black market. Giant drug distributors (like McKesson, Cardinal Health, and AmerisourceBergen) shipped millions of pills to tiny pharmacies in rural towns without scrutiny. For example, over a two-year period, nearly 9 million hydrocodone tablets were shipped to a single pharmacy in Kermit, West Virginia (population just 400 people); a colossal red flag that went ignored in the pursuit of profit. DEA officials later admitted they were slow to crack down on such rampant oversupply. Industry lobbying further neutered enforcement: in 2016, Congress (at the behest of pharmaceutical lobbyists) passed a law making it harder for the DEA to freeze suspicious opioid shipments, hobbling one of the agency’s key tools. In short, every institutional safeguard failed. State medical boards turned a blind eye to “pill mill” clinics pumping out prescriptions for cash. Politicians, courted by pharma money, were reluctant to impose strict limits on opioid prescribing until the crisis became undeniable. The oversight system that should have protected the public was effectively bought off or muzzled, clearing the way for opioid manufacturers and distributors to enrich themselves at the expense of American lives.
A Nation Awash in Pills (1999–2010)
Around 2010, belatedly, authorities began clamping down on the free-for-all of opioid prescribing. Law enforcement raided notorious pill mill clinics in states like Florida, shutting down sham pain clinics where lines of “patients” (many obviously addicted or diverting pills) stretched out the door. State governments implemented Prescription Drug Monitoring Programs to track opioid scripts and flag doctor-shopping. Purdue Pharma, under pressure, released a reformulated OxyContin in 2010 that was designed to be abuse-deterrent (harder to crush or dissolve for a quick high). The supply of prescription opioids finally tightened after a decade of glut. Prescriptions dropped by roughly 25% between 2012 and 2017 (5). This crackdown was necessary; but it had an unintended consequence that marked the second wave of the crisis. Thousands of people who had become addicted to prescription painkillers suddenly found those pills harder to get or too expensive. Cut off from one supply, they turned to a cheaper, readily available alternative: heroin.
Heroin, an illegal opioid, began flooding communities that had previously been hooked on OxyContin and Vicodin. By 2010, the U.S. saw a rapid rise in heroin overdose deaths, signaling this new phase (1). Mexican drug cartels seized the opportunity; they ramped up heroin production and distribution to meet the burgeoning demand from America’s prescription-opioid refugees. In fact, Mexican heroin output surged dramatically; increasing six-fold between 2005 and 2009; to feed the U.S. market (5). People who might never have imagined themselves injecting street heroin were now doing so, having first gotten addicted to opioid pills supplied by the pharmaceutical industry. Studies showed that roughly 4 out of 5 new heroin users had started by misusing prescription opioids (6). This is a damning statistic that directly links the overprescription of painkillers to the explosion of heroin use; the vast majority of heroin addicts in the 2010s began their opioid journey in a doctor’s office on supposedly “safe” meds (6). As pill supplies dried up, heroin was often easier and cheaper to obtain; a bag of heroin could be less costly than a single OxyContin tablet on the black market. By 2014, heroin had firmly entrenched itself in the suburbs and rural areas, not just the inner cities where it had long been present. Overdose deaths involving heroin tripled nationally from 2010 to 2015. Families that once faced a loved one’s prescription pill habit now faced the horror of heroin addiction, with all its associated dangers (injection-related diseases like HIV/hepatitis, risk of violent drug markets, etc.).
It’s important to note that this shift was entirely predictable; yet authorities did little to prepare. There was scant investment in addiction treatment or medication-assisted therapy to help those dependent on opioids. Instead of viewing the issue as a public health crisis, the system largely treated it as a law-and-order problem, cutting off the supply of pills and leaving addicted individuals to fend for themselves. Many ended up dead as a result. The crackdown on prescription opioids, while curbing new cases of painkiller addiction, left behind a generation of opioid-dependent people who simply migrated to illicit heroin. In essence, one type of opioid epidemic morphed into another. And an even deadlier twist was about to come.
Crackdown and the Shift to Heroin (2010–2013)
Around 2010, belatedly, authorities began clamping down on the free-for-all of opioid prescribing. Law enforcement raided notorious pill mill clinics in states like Florida, shutting down sham pain clinics where lines of “patients” (many obviously addicted or diverting pills) stretched out the door. State governments implemented Prescription Drug Monitoring Programs to track opioid scripts and flag doctor-shopping. Purdue Pharma, under pressure, released a reformulated OxyContin in 2010 that was designed to be abuse-deterrent (harder to crush or dissolve for a quick high). The supply of prescription opioids finally tightened after a decade of glut. Prescriptions dropped by roughly 25% between 2012 and 2017 (5). This crackdown was necessary – but it had an unintended consequence that marked the second wave of the crisis. Thousands of people who had become addicted to prescription painkillers suddenly found those pills harder to get or too expensive. Cut off from one supply, they turned to a cheaper, readily available alternative: heroin.
Heroin, an illegal opioid, began flooding communities that had previously been hooked on OxyContin and Vicodin. By 2010, the U.S. saw a rapid rise in heroin overdose deaths, signaling this new phase (1). Mexican drug cartels seized the opportunity: they ramped up heroin production and distribution to meet the burgeoning demand from America’s prescription-opioid refugees. In fact, Mexican heroin output surged dramatically – increasing six-fold between 2005 and 2009 – to feed the U.S. market (5). People who might never have imagined themselves injecting street heroin were now doing so, having first gotten addicted to opioid pills supplied by the pharmaceutical industry. Studies showed that roughly 4 out of 5 new heroin users had started by misusing prescription opioids (6). This is a damning statistic that directly links the overprescription of painkillers to the explosion of heroin use – the vast majority of heroin addicts in the 2010s began their opioid journey in a doctor’s office on supposedly “safe” meds (6). As pill supplies dried up, heroin was often easier and cheaper to obtain; a bag of heroin could be less costly than a single OxyContin tablet on the black market. By 2014, heroin had firmly entrenched itself in the suburbs and rural areas, not just the inner cities where it had long been present. Overdose deaths involving heroin tripled nationally from 2010 to 2015. Families that once faced a loved one’s prescription pill habit now faced the horror of heroin addiction, with all its associated dangers (injection-related diseases like HIV/hepatitis, risk of violent drug markets, etc.).
It’s important to note that this shift was entirely predictable – yet authorities did little to prepare. There was scant investment in addiction treatment or medication-assisted therapy to help those dependent on opioids. Instead of viewing the issue as a public health crisis, the system largely treated it as a law-and-order problem, cutting off the supply of pills and leaving addicted individuals to fend for themselves. Many ended up dead as a result. The crackdown on prescription opioids, while curbing new cases of painkiller addiction, left behind a generation of opioid-dependent people who simply migrated to illicit heroin. In essence, one type of opioid epidemic morphed into another. And an even deadlier twist was about to come.
The Rise of Illicit Fentanyl: A Third, Deadlier Wave

Just as the heroin surge was taking off, a new killer opioid entered the scene; one far more potent and insidious than the rest. Fentanyl, a synthetic opioid up to 50 times stronger than heroin, began appearing in the U.S. illicit drug supply around 2013. This signaled the start of the third wave of the opioid crisis (1). Initially, fentanyl was often mixed into heroin to boost its strength or pressed into counterfeit painkiller pills and sold to unwitting users. Because fentanyl is so powerful in tiny doses, these practices proved extraordinarily lethal. Overdose deaths skyrocketed yet again. From 2013 onward, the U.S. saw exponential increases in fatalities driven by illicit fentanyl and its analogues. By the late 2010s, synthetic opioids (primarily fentanyl) had become the number one cause of opioid overdose deaths, surpassing both prescription opioids and heroin. In 2022, fentanyl and its analogs were involved in an estimated two-thirds of all drug overdose deaths in America (2).
Why is fentanyl so deadly? As a lab-made drug, it can be produced cheaply and in massive quantities. Microgram-for-microgram, it delivers extreme potency; a few grains the size of salt can kill an adult. Traffickers embraced fentanyl because it is highly profitable and easier to smuggle (small packages can contain thousands of doses). But for users, it’s a game of Russian roulette: when someone buys a bag of heroin or a pill on the street today, it likely contains fentanyl, and the potency is wildly inconsistent. A dose they tolerate one day can silently be a fatal overdose the next. The result has been carnage. The period from 2015 to 2020 saw overall U.S. overdose deaths double, driven almost entirely by fentanyl infiltrating the drug supply. By 2021–2022, around 80,000 Americans were dying each year from opioid overdoses, with fentanyl responsible for the majority of those deaths (2). That is the equivalent of a 737 airplane full of people crashing every single day. The COVID-19 pandemic only worsened the trend, as isolation and disrupted treatment made many struggling individuals more vulnerable; 2020 and 2021 each set grim record highs for overdose fatalities. Although provisional data suggest deaths may have plateaued at this high level, the country is essentially enduring a 9/11-scale death toll from drugs every few weeks; year after year.
The influx of illicit fentanyl was not an accident of nature; it was engineered by drug trafficking enterprises exploiting America’s entrenched opioid demand. Early on, much of the illicit fentanyl was being manufactured in China and shipped directly to the U.S. via mail. Taking advantage of weak regulations and the anonymity of internet sales, Chinese chemical labs openly sold fentanyl powder and analogues to American customers or middlemen. The U.S. Drug Enforcement Administration confirmed that as of the mid-2010s, China was the primary source of illicit fentanyl flowing into the United States (8). In response to U.S. pressure, China nominally banned fentanyl and its core analogues in 2019, but clever chemists simply shifted to manufacturing precursor chemicals and novel analogues not on the banned list. These precursors are the ingredients needed to make fentanyl, and they soon began flowing in huge volumes to Mexico.
The Global Supply Chain: Chinese Labs and Mexican Cartels

Behind the surge of street fentanyl lies a global network of profit-driven criminals who stepped in to supply opioids after U.S. corporations’ pill gravy train slowed. Chinese chemical manufacturers and Mexican drug cartels became key players, effectively partnering (albeit at arm’s length) to keep Americans drowning in cheap, deadly opioids. As one U.S. official bluntly put it, “the global fentanyl supply chain, which ends with the deaths of Americans, often starts with chemical companies in China” (7). These Chinese firms, operating with impunity, mass-produce fentanyl precursors and even finished fentanyl, then sell them through black-market channels. According to the DEA, Chinese chemical companies are “fueling the fentanyl crisis” in the United States by sending fentanyl precursors and analogues in enormous quantities, either directly or via Mexico (7). Shipments of these chemicals are frequently mislabeled and routed through various countries to evade detection. Despite diplomatic efforts, China’s enforcement against these outlaw labs has been minimal; likely because these companies make money and the casualties are an ocean away.
On the receiving end of those precursor chemicals, Mexico’s major drug cartels have built a booming fentanyl manufacturing and trafficking operation. The Sinaloa Cartel (formerly helmed by Joaquín “El Chapo” Guzmán and now partly run by his sons) and the Jalisco New Generation Cartel (CJNG) are the two dominant players. They have established clandestine labs in Mexico that can churn out fentanyl by the kilo, which is then pressed into millions of fake pills (often made to look like Xanax, Percocet or other popular meds) or mixed into batches of heroin, cocaine, and even stimulants. The DEA reports that the Sinaloa and CJNG cartels are the primary groups responsible for flooding the U.S. with illicit fentanyl; nearly every significant fentanyl seizure or lab bust can be traced back to these organizations (8). These cartels have capitalized on fentanyl because it is far more profitable than plant-based drugs. Whereas heroin requires hectares of poppy cultivation and a large workforce, fentanyl can be cooked in an industrial vat anywhere. The cartels’ business model is straightforward: produce mass quantities of fentanyl-laced pills for pennies per pill, and smuggle them into the U.S. hidden among legal commerce or carried by drug mules. From 2018 onward, U.S. authorities have interdicted shocking amounts of fentanyl at the southern border; multi-kilogram loads, each kilogram containing half a million lethal doses. In just a few months in 2022, the DEA seized over 10 million fentanyl pills and almost a thousand pounds of fentanyl powder, which combined equated to hundreds of millions of potentially fatal doses removed from circulation. This gives a sense of the scale of product the cartels are pushing into the country. Undoubtedly, much more gets through, and is sold on street corners from Los Angeles to Boston. The cartels have shown complete disregard for the lives lost; for them, every American who develops a fentanyl habit is simply a repeat customer (until they overdose and die, at which point the dealers move on to the next victim). The partnership of Chinese chemical suppliers and Mexican trafficking networks ensured that when America tried to clamp down on one opioid source (pills), an even deadlier source took its place; truly pouring gasoline on the fire that U.S. pharma ignited.
Communities Devastated: Homelessness, Orphans, and Urban Decay
After more than two decades, the opioid crisis has left an appalling trail of human wreckage. This public health disaster has deeply scarred the social fabric of America. Consider the families: hundreds of thousands of parents have lost children to opioid overdoses, and many thousands of children have lost parents. An entire generation of Americans has grown up during this epidemic; in some communities, attending multiple funerals for classmates or neighbors who overdosed became distressingly routine. In the hardest-hit areas, the local economies and way of life have been upended. Factories and coal mines closed in parts of Appalachia right as OxyContin swept through, leading to a vicious cycle of joblessness and addiction. Indeed, research has linked opioid prevalence to drops in labor force participation; people in their prime working years incapacitated by addiction (1). And when breadwinners succumb to drugs, their families often fall into poverty or disintegrate. Many grandparents unexpectedly became primary caregivers to grandchildren because the middle generation was wiped out by opioids. Child welfare systems overflowed with kids whose parents were addicted or dead. The foster care rolls swelled in many states as the crisis peaked.
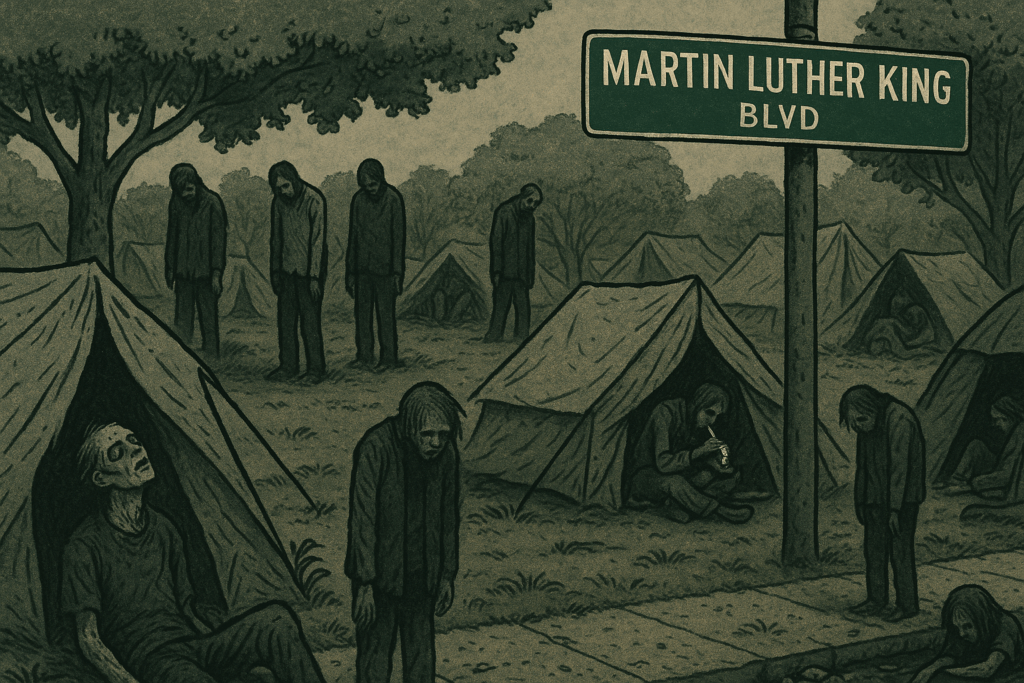
In U.S. cities, one of the most visible signs of the opioid plague is the surge in homelessness and open-air drug use. Urban neighborhoods like Kensington in Philadelphia have become notorious as lawless heroin/fentanyl encampments, resembling something out of a post-apocalyptic film. The streets of Kensington are lined with dozens of emaciated, addicted individuals huddled around barrel fires, tents and makeshift shelters crowding the sidewalks, needles and trash littering the ground. The area has been dubbed the East Coast’s largest open-air drug market, a place where the opioid and now fentanyl crisis is on full display at all hours. An estimated 75% of people living unsheltered in the Kensington neighborhood suffer from substance use disorder, primarily opioid addiction (11). Similar scenes play out on the West Coast: parts of San Francisco’s Tenderloin district or Los Angeles’s skid row have seen an influx of fentanyl, contributing to spikes in overdoses among the homeless population. Nationwide, the interplay between homelessness and the opioid epidemic is profound. Studies have found that homelessness itself greatly increases the risk of drug overdose death; one analysis showed that a mere 10% reduction in the homeless population could save over 650 lives a year from opioid overdoses, while a 25% reduction could save nearly 2,000 lives (9). In other words, the opioid crisis and the housing crisis are feeding one another, creating a deadly feedback loop (homelessness exacerbates addiction, and addiction in turn causes homelessness).
Beyond the human toll, entire communities have been gutted by opioids. Small towns in West Virginia, Ohio, and Kentucky lost so many residents to overdose or drug-related decay that they are a shell of what they once were. In some counties, ambulance crews have reversed more overdoses with Narcan than they transport heart attack victims; a grim new normal straining local resources. Businesses in affected downtowns struggle to survive amid the crime and disorder accompanying heavy drug use; many storefronts stand vacant. Public spaces; parks, libraries, transit stations; have at times become hazard zones with frequent overdoses and drug dealing in plain sight, discouraging general public use and eroding quality of life. The crisis also placed an immense burden on healthcare systems: hospitals saw soaring admissions for overdose, endocarditis (a heart infection common in IV drug users), and other complications; coroners’ offices ran out of space for the bodies. The economic cost of the opioid epidemic is almost incalculable; factoring health care, law enforcement, lost productivity, and societal costs, a Congressional analysis estimated the cost at $1.5 trillion for just the year 2020 (10). Cumulatively, some studies put the economic burden in the multiple trillions over the past decade. But even these staggering dollar figures pale in comparison to the incalculable human cost; the trauma and grief of millions of families, the neighborhoods plunged into despair, the potential and promise of so many lives cut short.
Profit and Power: Incentives Behind the Carnage
How did this disaster happen in an advanced nation with regulatory agencies and a sophisticated healthcare system? The blunt answer: every key actor’s incentives were aligned toward making money or gaining power at the expense of public health. The opioid crisis is a case study in perverse incentives and moral failures. It started with pharmaceutical companies like Purdue, whose incentive was simple: profit above all. The Sackler family and Purdue’s executives knew that turning OxyContin into a blockbuster would make them fabulously wealthy. So they deliberately expanded the opioid market; pushing opioids for chronic ailments, downplaying risks, and even blaming patients when they became addicted (Purdue infamously coined the term “pseudoaddiction,” claiming that apparent drug-seeking was actually undertreatment of pain requiring more opioids). This was greed in its purest form. Internal emails revealed callous strategies, like one Sackler executive suggesting they “hammer on the abusers” as reckless criminals to deflect blame from the drug and company. The billions the Sacklers pocketed (over $10 billion withdrawn from Purdue, as noted) were essentially blood money earned by spreading addiction (12). Other drug companies (Johnson & Johnson, Endo, Teva, Mallinckrodt, etc.) joined the fray with their own opioids or by supplying raw ingredients, all profiting from increased opioid sales. For the drug makers, more prescriptions meant more revenue; any downside was someone else’s problem.
Next are the regulators and government agencies. Agencies like the FDA had an incentive (or at least strong pressure) to approve new pain drugs and not stifle the pharmaceutical industry; in part because of industry influence and a political climate favoring faster drug approvals. The FDA gets significant funding from industry user fees, which critics say can make it “client-friendly” toward the companies it regulates. Their leaders likely feared political blowback or lawsuits if they limited access to pain treatment. Whatever the case, the FDA’s failure to act suggests that protecting consumers was not prioritized over keeping industry happy. The DEA and big distributors also had skewed incentives: for distributors, shipping more pills meant more profit, and their executives often earned bonuses based on sales volume. They had every reason not to look too hard at suspicious orders. The DEA, for its part, faced internal and external pressure to balance enforcement with ensuring medications for pain were available; a balance they disastrously mismanaged on the lenient side. Some DEA officials later took jobs in the pharmaceutical sector, raising questions of revolving-door incentives.
Many doctors and pharmacies were likewise swept up by perverse incentives. Most physicians certainly didn’t intend harm; they were reassured by Purdue’s information that opioids were safe, and they wanted to alleviate pain (and in America’s fee-for-service system, writing a prescription is quick and reimbursed, whereas spending time on complex pain management is not). Pill mill doctors, however, were outright drug dealers in lab coats, motivated by easy cash from churning through dozens of patients a day and writing high-dose opioid scripts for anyone who could pay. Small-town pharmacies in places like West Virginia saw their business boom by dispensing huge volumes of opioids; owners often looked the other way and enjoyed the profits. Corporate pharmacy chains also benefited from increased traffic and sales. Until lawsuits and public outrage forced their hand, they had little financial incentive to question high opioid prescription rates; to do so might mean losing customers to a competitor.
When the crisis shifted to illicit drugs, the incentives driving the devastation remained just as ruthless. Mexican cartels are motivated by profit and power. For them, fentanyl is a godsend: they can produce it cheaply without relying on crop cycles, and it creates strong physiological dependency in users (meaning returning customers). The calculus is cold-blooded: even if fentanyl kills a chunk of their client base, there will always be new users coming up; and the profit margins are so high that it offsets the loss. In fact, some cartel factions weaponized fentanyl as a strategy to expand market share, flooding areas with super-potent product to eliminate competition, heedless of the overdose deaths caused. The Chinese chemical suppliers are similarly money-driven. Often operating in a gray area of Chinese law, these companies and brokers make enormous sums supplying precursors. There is virtually no consequence for them since they operate abroad; thus their incentive is purely to sell more chemicals. Some have even marketed new fentanyl analogues with slogans about how potent or effective they are; acting as pseudo-pharma companies with zero regulation.
Even at the level of governance and policy, incentives were misaligned or politics got in the way. For years, some lawmakers were reluctant to crack down hard on opioid manufacturers or fund treatment programs; campaign donations from pharma and a general ideological resistance to government intervention played a role. The result was a toothless initial response. Only once the crisis became a national scandal did politicians pivot, by which time it was too late to prevent the cascade of heroin and fentanyl. Meanwhile, early victims of the opioid surge were often working-class, rural, or otherwise marginalized communities, and one cannot ignore that there was likely a lack of urgency in the halls of power because of who was suffering (had the early wave been Wall Street bankers dying en masse, the response might have been more swift). In short, no one with the power to stop the opioid epidemic had a strong enough incentive to do so at the time it mattered. Corporations wanted money, regulators didn’t want to upset corporate interests, traffickers wanted to create and supply more addicts, and the victims; everyday Americans struggling with pain or addiction; had little voice or influence. By the time the alarms rang loud, millions were already hooked and hundreds of thousands were dead. This was not a well-meaning policy gone awry or a tragic unforeseen side effect; it was the predictable outcome when profit and greed override ethics at every step.
Conclusion: A Catastrophe with Clear Villains
The U.S. opioid crisis did not have to happen; it was the result of deliberate actions (and deliberate inactions) by identifiable actors. In a just world, these actors would face harsh accountability for the lives destroyed. The pharmaceutical executives who cynically marketed opioids as safe, the Sackler family that built a dynasty of wealth by igniting mass addiction, the FDA officials and policymakers who fell under the sway of industry or failed to do their due diligence, the distributors and pharmacies that turned a blind eye to blatant drug diversion, and the foreign crime syndicates that pumped lethal poison into vulnerable communities; all of them share blame for an American tragedy. Together, they transformed the landscape of American public health, creating what the CDC has called the worst drug epidemic in our history (1). The numbers speak to a historic calamity: over 700,000 opioid overdose deaths since 1999 (2), overall drug fatalities topping 100,000 per year, life expectancy in the U.S. declining in recent years largely due to these deaths. But beyond the numbers are the stories; millions of individuals suffering from addiction, families shattered by grief, towns and cities plunged into an interminable nightmare of funeral vigils and emergency sirens.
What sets the opioid epidemic apart is that it was manufactured for profit. This wasn’t an accident or an epidemic that emerged organically; it was driven by greed every step of the way. We must be unequivocal on this point: the crisis was man-made. The “opioid plague” did not descend upon America randomly; it was ushered in by the pharmaceutical industry’s lies and stoked by systemic failures and illicit profiteering. It’s a cautionary tale of what happens when corporate power, regulatory weakness, and illicit enterprise collide. Even today, as we grapple with the fentanyl era, those same forces remain in play. The institutions meant to protect the public must reckon with their abdication of responsibility. And society at large must contend with the aftermath; an entire generation scarred, and communities that will take decades to recover, if they ever do.
There is nothing abstract about the devastation: one can walk through certain neighborhoods in West Virginia, Ohio, Pennsylvania, or California and see the hollowed-out houses, the memorials in church yards, the faces of children growing up without parents. The opioid crisis is as real and as ugly as it gets. And it was made possible by named individuals and organizations that chose profit, expediency, or indifference over human life. Any attempt to sugarcoat this reality would be an insult to the victims. The United States is only now starting to hold some of these parties to account through lawsuits and settlements (billions in damages have been levied, Purdue Pharma was forced into bankruptcy, some cartel leaders have been indicted). But no amount of money can truly compensate for the scale of harm done. The opioid crisis will forever remain a dark stain on America’s recent history; a lethal convergence of avarice and ineptitude that unleashed untold suffering. It stands as a stark lesson that when corporate and government institutions betray the public trust, the consequences can be catastrophic. And it demands that we remain unflinchingly critical of those whose actions; or failures to act; lead to such colossal loss of life.
Sources:
- Kolodny, Andrew. “How FDA Failures Contributed to the Opioid Crisis.” AMA Journal of Ethics, vol. 22, no. 8, Aug. 2020. (Includes quotes from a federal judge calling the opioid epidemic a “man-made plague” and cites inadequate FDA oversight as a cause of the crisis.)
- Ferragamo, Mariel, and Claire Klobucista. “Fentanyl and the U.S. Opioid Epidemic.” Council on Foreign Relations Backgrounder, updated 28 Mar. 2025. (Provides an overview of the opioid crisis, noting over one million overdose deaths since 2000 and that recent fatalities are largely driven by fentanyl, with most supply coming from China and Mexico.)
- Zarroli, Jim. “OxyContin Addiction Case Yields Millions in Fines.” NPR News, 10 May 2007. (Reports on Purdue Pharma’s 2007 guilty plea for misbranding OxyContin; includes U.S. Attorney John Brownlee’s statement that OxyContin was “the child of marketers and bottom-line financial decision-making,” and details how Purdue misled doctors about addiction risks.)
- Van Zee, Art. “The Promotion and Marketing of OxyContin: Commercial Triumph, Public Health Tragedy.” American Journal of Public Health, vol. 99, no. 2, Feb. 2009. (Documents Purdue’s aggressive marketing of OxyContin, noting sales grew from $48 million in 1996 to $1.1 billion in 2000, and that OxyContin became a leading drug of abuse by 2004. Also discusses the FDA-approved labeling that claimed addiction was “very rare” and that OxyContin’s delayed release reduced abuse potential – statements removed in 2001 as evidence of abuse mounted.)
- National Institute on Drug Abuse (NIDA). “Prescription Opioids and Heroin Research Report: Increased drug availability is associated with increased use and overdose.” NIDA/NIH, accessed 2022. (Explains that opioid prescriptions dispensed by U.S. pharmacies more than tripled from 76 million in 1991 to 255 million in 2012, and that in parallel, opioid-involved overdose deaths quadrupled. Also notes a decline in prescriptions to ~143 million by 2020 after reforms.)
- National Institute on Drug Abuse (NIDA). “Prescription Opioids DrugFacts.” NIDA/NIH, revised 2020. (States that about 80% of people who use heroin first misused prescription opioids. This data illustrates the progression from prescription opioid abuse to heroin use for a large share of individuals, highlighting how the crackdowns on pills led to a shift toward heroin.)
- U.S. Department of Justice – Office of Public Affairs. “Justice Department Announces Eight Indictments Against China-Based Chemical Manufacturing Companies and Employees.” Press Release, 3 Oct. 2023. (Quotes Attorney General Merrick Garland and DEA Administrator Anne Milgram on Chinese companies fueling the fentanyl crisis by exporting precursor chemicals and analogues. Milgram explicitly says, “Chinese chemical companies are fueling the fentanyl crisis in the United States by sending fentanyl precursors… into our country and into Mexico,” underscoring China’s role in the supply chain.)
- U.S. Drug Enforcement Administration (DEA). DEA Intelligence Report: Fentanyl Flow to the United States. Published March 2020. (Details how Mexico and China are the primary sources of illicit fentanyl. Notes that Mexican transnational criminal organizations, specifically the Sinaloa Cartel and Jalisco New Generation Cartel, are the primary trafficking groups responsible for smuggling fentanyl into the U.S., either by producing it in Mexico using precursors from China or distributing finished fentanyl from China.)
- Hataway, Leigh. “Homelessness leads to more drug, alcohol poisoning deaths.” UGA Today (University of Georgia News), 5 Feb. 2024. (Summarizes a study published in Health Affairs. Finds that higher homelessness rates are associated with higher overdose death rates. Notably, it